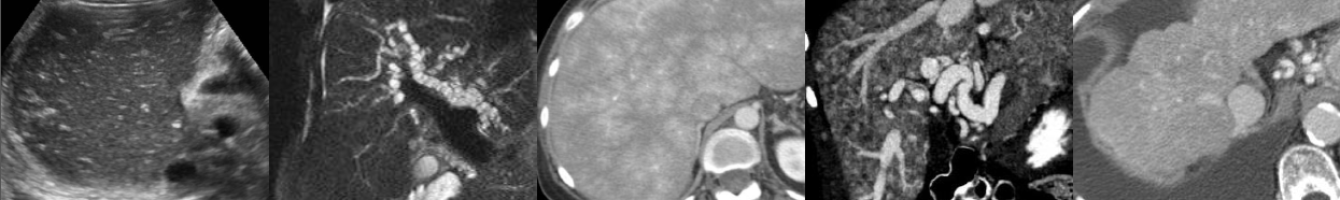
Non-masslike Adrenal Abnormalities
In this video lecture, we discuss the normal imaging appearance of the adrenal glands, as well as multiple common and rare non-masslike adrenal abnormalities on CT and MRI.
Key points include:
- The adrenal glands normally have an inverted “V” or “Y” configuration.
- A linear, disk-like adrenal gland or “pancake” adrenal gland indicates congenital malposition or absence of the ipsilateral kidney.
- Adrenal hyperenhancement raises suspicion for developing shock and may signal a therapeutic window to act upon.
- Adrenal calcifications can be caused by prior hemorrhage, infection, tumors and metabolic syndromes.
- On MRI, T1-weighted in-phase GRE images can be helpful in identifying calcification due to dark blooming caused by susceptibility artifact.
- Adrenal atrophy may indicate adrenal insufficiency.
- Adrenal hyperplasia is identified when adrenal limbs measure greater than 10 mm in thickness and may or may not be hormonally functioning.
- Nonhemorrhagic adrenal infarction appears as a nonenhancing, edematous adrenal gland with surrounding stranding and restricted diffusion.
- Adrenal infarction can be seen in hypercoagulable states, antiphospholipid-antibody syndrome and pregnancy.
Podcast: Play in new window | Download
Subscribe: Email