GU – Adrenal
- Update on CT and MRI of Adrenal Nodules Key Points
“For example, approximately one-third of pheochromocytomas will show washout in the adenoma range, and adenomas can enhance avidly on the 70-second phase of enhancement [52–55]. Therefore, pheochromocytomas cannot be reliably differentiated from adenomas using CT washout protocols [52–55] (Fig. 7). The presence of intracytoplasmic lipid effectively excludes the diagnosis of pheochromocytoma [55] because this finding has been described in only two previous case reports [72, 73]. “
- Comparison of Quantitative MRI and CT Washout Analysis for Differentiation of Adrenal Pheochromocytoma From Adrenal Adenoma Key Points
“In our study, no pheochromocytoma contained intracellular lipid according to previously described quantitative unenhanced CT (< 10 HU) or chemical-shift MRI (chemical-shift SI index > 16.5%, adrenal-to-spleen SI ratio < 0.71) thresholds.”
“The presence of intracellular lipid in adrenal pheochromocytoma is extraordinarily rare. Only two case reports [14, 33] have been published to date in the histopathologic and imaging literature.”
“Only one pheochromocytoma has been found to have unenhanced CT attenuation less than 10 HU [14], and to our knowledge, there has been no report of a pheochromocytoma exhibiting intracellular lipid on chemical-shift MR images. It can therefore be concluded that the presence of intracellular lipid in an incidental adrenal nodule is nearly diagnostic of adrenal adenoma.”
“In lesions larger than 4 cm or in patients with a known malignancy, intracellular lipid should be interpreted more cautiously. Both adrenal cortical carcinoma and metastases (from lipid-containing primary tumors, such as renal cell carcinoma or hepatocellular cell carcinoma) must also be considered in the differential diagnosis because these lesions can mimic adenoma on the basis of quantitative imaging thresholds alone [7].”
- Can Established CT Attenuation and Washout Criteria for Adrenal Adenoma Accurately Exclude Pheochromocytoma? Key Points
“A substantial minority of pheochromocytomas have absolute or relative washout characteristics that overlap with those of lipid-poor adenomas.”
“None of the pheochromocytomas had an unenhanced attenuation of 10 HU or less.”
“Blake et al. [14] reported a series of nine adrenal nodules producing “pheochromocytoma syndrome,” in which one histologically confirmed pheochromocytoma showed both absolute washout greater than 60% and an unenhanced attenuation less than 10 HU. The authors concluded that pheochromocytoma should be included in the differential diagnosis of nodules meeting washout or attenuation criteria for adrenal adenoma. Our results agree with these findings, although none of the 38 pheochromocytomas imaged with un-enhanced CT in our series would have been confused for a lipid-rich adenoma, because none of these lesions had an unenhanced attenuation value less than or equal to 10 HU (our study minimum was 15 HU).”
- MDCT of Adrenal Masses: Can Dual-Phase Enhancement Patterns Be Used to Differentiate Adenoma and Pheochromocytoma? Key Points
“For indeterminate adrenal masses identified at dual-phase IV contrast-enhanced CT, higher enhancement during the arterial phase, arterial phase enhancement levels greater than 110 HU, and lesion heterogeneity should prompt consideration of pheochromocytoma.”
“The sensitivity of 110-HU arterial enhancement for pheochromocytoma was 58%, the specificity was 100%, the positive predictive value was 100%, and the negative predictive value was 89%.”
“No adenoma was more than 85-HU enhancing in the arterial phase, and 58% of pheochromocytomas were more than 110-HU enhancing. Most adenomas (85%) were more enhancing in the venous phase.”
“Venous phase enhancement greater than 110 HU was identified in 7% (3/41) of adenomas.”
- Adrenal Masses: Characterization with Combined Unenhanced and Delayed Enhanced CT
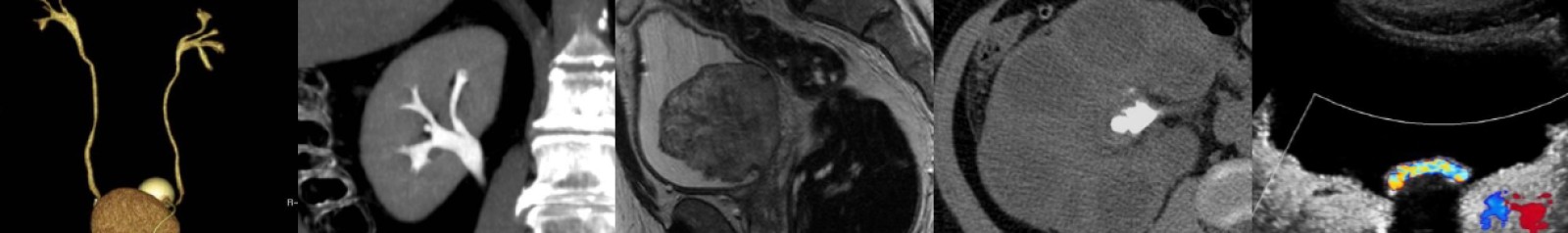
- Pheochromocytoma: An Imaging Chameleon