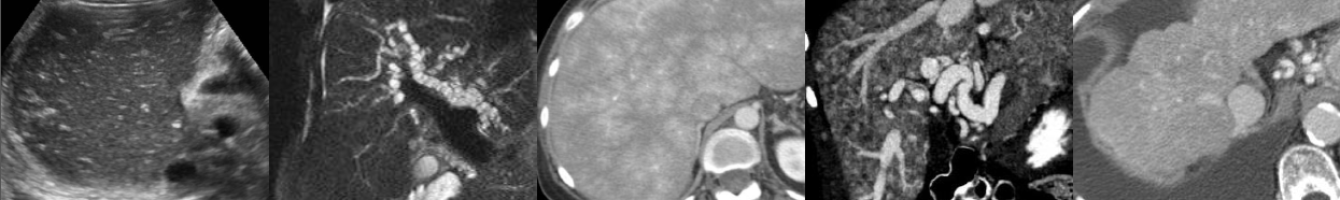
Introduction to Multiphase CT & MRI of the Liver
In this video lecture, we review the appearance of the liver on multiphase CT & MRI. A basic approach to image interpretation is presented with pitfalls to avoid.
Key points include:
- The three major liver postcontrast phases include the late hepatic arterial phase, portal venous phase, and delayed/equilibrium phases.
- The hepatic artery enhances first, followed by the portal veins, then the hepatic veins along with the hepatic parenchyma.
- An ideal late hepatic arterial phase sequence will have both hepatic artery and portal vein enhancement with no hepatic vein enhancement.
- The late hepatic arterial phase occurs at about the same time as the corticomedullary phase, enteric phase, pancreatic phase, and splenic arciform enhancement phase.
- The early arterial phase of an angiographic CT is NOT the same as the late hepatic arterial phase of a liver protocol study and may be too early to adequately assess hypervascular liver lesions.
- “MRI CT” is a handy mnemonic for hypervascular liver metastases, lesions that will be best detected on a hepatic arterial phase series.
- Portal venous phase images will have portal vein and hepatic vein enhancement, as well as liver parenchymal enhancement.
- Hypovascular hepatic metastases (GI tract, pancreas) are usually best detected on the portal venous phase.
- Delayed/equilibrium phase images allow detection of intralesional contrast washout and delayed capsular enhancement typical of hepatocellular carcinoma, as well as evaluation of delayed enhancement as seen with hemangiomas and intrahepatic cholangiocarcinoma.
- CT has better spatial resolution, but MRI has better contrast resolution and is therefore superior to CT in the characterization of liver masses.
- Pre- and postcontrast MRI sequences are typically obtained as a special T1 sequence known as a spoiled 3D gradient echo variant with fat saturation.
Podcast: Play in new window | Download
Subscribe: Email