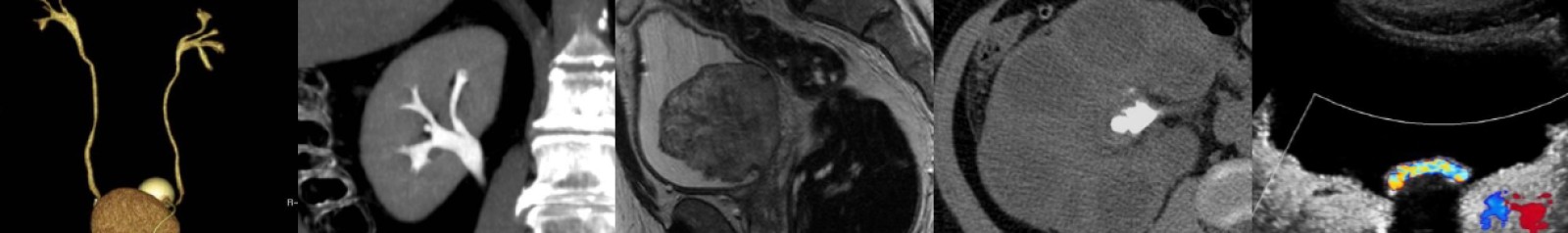
Hepatic Hemangioma: Pitfalls & Mimics, Part I
In this video lecture, we discuss tips and tricks to diagnose everybody’s favorite hepatic tumor on CT, MRI and ultrasound.
Key points include:
- Hemangioma is the most common benign hepatic tumor, and it is more common in females.
- These tumors are usually asymptomatic and typically require no treatment, but can rarely cause pain, rupture if large, or cause Kasabach-Merritt syndrome.
- On nonenhanced CT, hemangiomas will be hypodense to liver parenchyma and homogeneously isodense to the blood pool.
- There are three major enhancement patterns for typical hemangiomas, and all patterns will show persistent delayed enhancement without contrast washout.
- Peripheral, nodular, interrupted enhancement with gradual centripetal progression to uniform enhancement is the most common pattern.
- Smaller lesions (less than 1-2 cm) can have immediate uniform enhancement and appear flash-filling.
- Larger hemangiomas may have a central scar that does not enhance.
- MRI is highly specific in the diagnosis of hemangioma.
- On MRI, hemangiomas will appear T1 hypointense and T2 hyperintense to liver parenchyma, or (perhaps more importantly) T1 isointense to the blood pool and T2 hyperintense to the spleen.
- Hemangiomas usually do not show restricted diffusion.
- If present, the central scar of hemangioma will appear T1 hypointense and T2 hyperintense on MRI.
- Additional liver masses that may have a central scar include focal nodular hyperplasia, fibrolamellar hepatocellular carcinoma, cholangiocarcinoma, and hepatocellular carcinoma.
- On ultrasound, hemangiomas are usually uniformly echogenic.
- 40% of hemangiomas can have a “reverse target” appearance with an echogenic periphery and hypoechoic center.
- Hemangiomas usually have no color Doppler flow on ultrasound, but they may occasionally exhibit mild flow.
Podcast: Play in new window | Download
Subscribe: Email