GU – Renal Masses
- Enhancement Threshold of Small (< 4 cm) Solid Renal Masses on CT Key Points
“A minority of small RCCs do not reach either a 15- or 20-HU enhancement threshold and might be misinterpreted as a hyperattenuating cyst. Most RCCs below these enhancement thresholds are papillary RCC.”
- Prevalence of Solid Tumors in Incidentally Detected Homogeneous Renal Masses Measuring > 20 HU on Portal Venous Phase CT Key Points
“Our findings suggest that the most appropriate attenuation value cutoff for recommending follow-up imaging of small homogeneous renal masses may be higher than 20 HU. Although we found no solid masses in the 20- to 40-HU range, the number of lesions in the 30- to 40-HU range was smaller.”
“We suggest that small homogeneous renal masses measuring < 30 HU require no further follow-up.”
“Our mean lesion size was 16 mm, and more than two-thirds were either entirely surrounded by renal parenchyma or were < 50% exophytic. Thus, many of the lesions in our study were at risk of pseudoenhancement. Our findings may not apply to larger, more exophytic masses, and it is prudent to assess the risks of pseudoenhancement on a case by case basis.”
“Small indeterminate homogeneous renal masses measuring 20–40 HU on portal venous phase CT images are highly likely to be benign cysts. Follow-up of lesions measuring < 30 HU may not be warranted.”
- How I Do It: Evaluating Renal Masses
- Pitfalls in Renal Mass Evaluation and How to Avoid Them
- A Practical Approach to the Cystic Renal Mass
- Evaluation of Bosniak category IIF complex renal cysts (Table 2)
- Infiltrative Renal Lesions: Radiologic-Pathologic Correlation
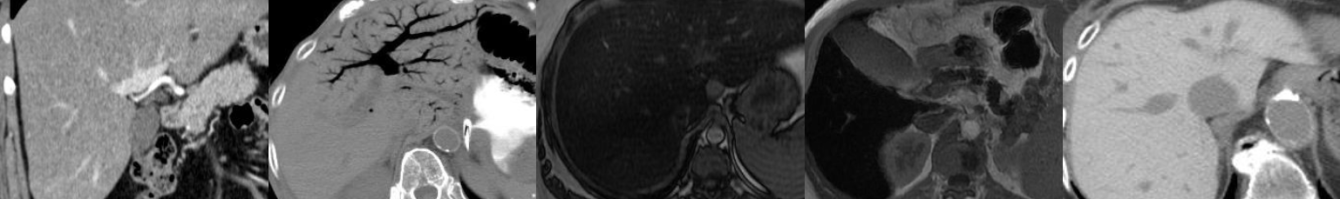
- Common and Uncommon Histologic Subtypes of Renal Cell Carcinoma: Imaging Spectrum with Pathologic Correlation
- Differentiation of Subtypes of Renal Cell Carcinoma on Helical CT Scans Key Points
“According to the First International Workshop on Renal Cell Carcinoma held by the World Health Organization, renal cell carcinoma can be classified into conventional (i.e., clear cell) renal carcinoma, papillary renal carcinoma, chromophobe renal carcinoma, collecting duct renal carcinoma, and unclassified renal carcinoma.”
“Conventional renal carcinoma is the most common subtype, accounting for approximately 70% of renal cell carcinomas; the overall 5-year survival rate of patients with conventional renal carcinoma ranges from 55% to 60%. Papillary renal carcinoma, the second most common subtype, comprises from 15% to 20% of renal cell carcinomas and is associated with a high 5-year survival rate (80-90%).”
“Conventional renal carcinoma showed stronger enhancement than nonconventional renal carcinomas in both the corticomedullary and excretory phases, and the tumors that enhanced more than approximately 84 H in the corticomedullary phase and 44 H in the excretory phase were likely to be conventional renal carcinoma.”
“Chromophobe renal carcinoma…tends to exhibit homogeneous enhancement on CT. Conventional renal carcinoma…usually shows heterogeneous or predominantly peripheral enhancement on CT.”
“A tumor that is greater than 7 cm in diameter, exhibits homogeneously weak enhancement, and has calcifications is strongly suggestive of chromophobe renal carcinoma.”
“In addition, a tumor with heterogeneously strong enhancement and a diameter of less than 3 cm may indicate conventional renal carcinoma.”
“Calcification was more common in papillary and chromophobe renal carcinomas than in conventional renal carcinoma.”
“Perinephric change and venous invasion were not noted in chromophobe renal carcinoma, whereas both were common in collecting duct renal carcinoma.”
“Hemorrhage and necrosis are predictors of poor prognosis, and calcification suggests a higher 5-year survival rate. Hemorrhage and necrosis (heterogeneous or predominantly peripheral enhancement pattern) were more common in conventional and collecting duct renal carcinomas, both of which are associated with a poor prognosis. Calcification was more frequently seen in papillary and chromophobe renal carcinomas, which are associated with a better prognosis.”
“A patient with a subtype of renal cell carcinoma that tends to not metastasize, such as chromophobe renal carcinoma, may not need to undergo a complex metastasis survey. An unnecessarily wide resection may be avoided in patients with a subtype that is unlikely to recur or metastasize, thereby reducing postoperative morbidity and mortality.”
- Delayed CT to Evaluate Renal Masses Incidentally Discovered at Contrast-enhanced CT: Demonstration of Vascularity with Deenhancement Key Points
“Delayed CT of incidentally discovered well-demarcated homogeneous high-attenuating (>30-HU) renal masses detected at postcontrast CT enables differentiation of high-density cysts from renal neoplasms by demonstrating deenhancement as a proof of vascularity and, hence, neoplasm.”
“In the masses that demonstrated deenhancement, the mean difference in attenuation values between the initial postcontrast and delayed CT studies was 32.3 HU (range, 15–67 HU).”
“There is no absolute number of Hounsfield units that can be used to signify enhancement or deenhancement. What is needed is an understanding of the possible pitfalls involved in these measurements so that the necessary adjustments can be made. Whatever the value of tissue enhancement or deenhancement used, it must be stressed that enhancement or deenhancement must be unequivocal to be used in the diagnosis.”
- Imaging of Renal Lymphoma: Patterns of Disease with Pathologic Correlation