Imaging of Pheochromocytoma
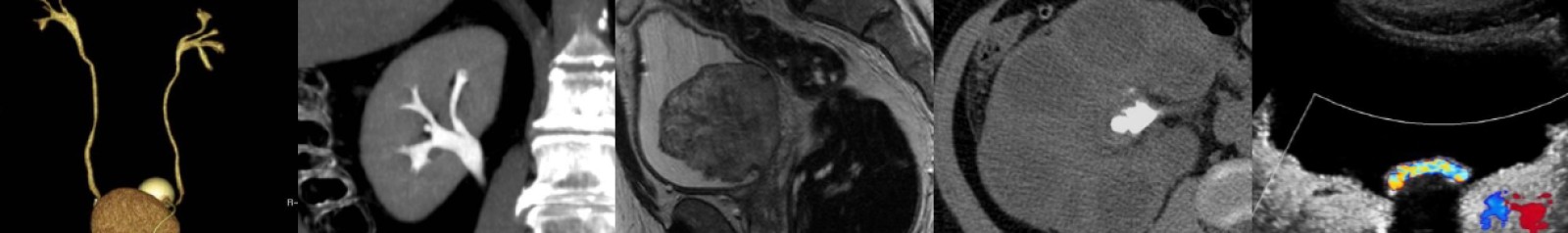
In this video lecture, we discuss the diagnosis and imaging appearance of pheochromocytoma on ultrasound, CT, MRI, and nuclear medicine studies.
Key points include:
- Pheochromocytoma is a biochemical diagnosis.
- Symptoms are variable, and patients may present with headache, palpitations, sweating, hypertension or be asymptomatic.
- Most cases are sporadic with mean age of presentation in the 40s.
- Hereditary pheochromocytoma can be seen in the setting of Von Hippel-Lindau disease, multiple endocrine neoplasia (MEN) type II, neurofibromatosis type I, and pheochromocytoma-paraganglioma syndromes associated with succinate dehydrogenase gene mutations.
- Pheochromocytoma is the “10%” tumor, as approximately 10% are bilateral, extra-adrenal, contain calcification, occur in children, or are malignant.
- Most pheochromocytomas are solid, but they can also appear as mixed cystic and solid with varying degrees of complexity.
- The ultrasound appearance is nonspecific, and tumors may contain echogenic hemorrhage or be hypervascular on Doppler imaging.
- Any mass that enhances to a density greater than 110 HU on an arterial phase CT scan should raise suspicion for pheochromocytoma.
- On CT, most pheochromocytomas will have noncontrast density greater than 10 HU and absolute washout less than 60%, findings similar to adrenal metastases and adrenocortical carcinoma.
- However, pheochromocytoma can rarely have noncontrast density less than 10 HU and absolute washout greater than 60%, thus mimicking adrenal adenoma.
- Studies have shown that pheochromocytoma is not a contraindication to modern nonionic IV contrast media.
- On MRI, the “light bulb” T2 bright appearance classically associated with pheochromocytoma may or may not be present.
- If intratumoral hemorrhage is present, pheochromocytomas may show T1 hyperintensity or susceptibility artifact on T1-weighted in-phase images depending on the age of blood.
- Pheochromocytomas usually do not show signal dropout on T1-weighted opposed-phase images but rarely do and can mimic adrenal adenomas.
- MIBG scans have nearly 100% specificity for pheochromocytoma and are useful to confirm clinically suspected pheochromocytoma and for detection of metastatic disease.
- Extra-adrenal pheochromocytomas (paragangliomas) usually occur in abdomen, typically at the organ of Zuckerkandl or in the retroperitoneum.
Podcast: Play in new window | Download
Subscribe: Email