GI – Pancreas
- Cystic Pancreatic Lesions: A Simple Imaging-based Classification System for Guiding Management Key Points
“Pseudocysts, serous cystadenomas, mucinous cystic neoplasms, and IPMNs are most often encountered in routine practice, accounting for more than 90% of cystic pancreatic lesions. Pseudocysts typically occur with acute pancreatitis or may develop insidiously in the setting of chronic pancreatitis.”
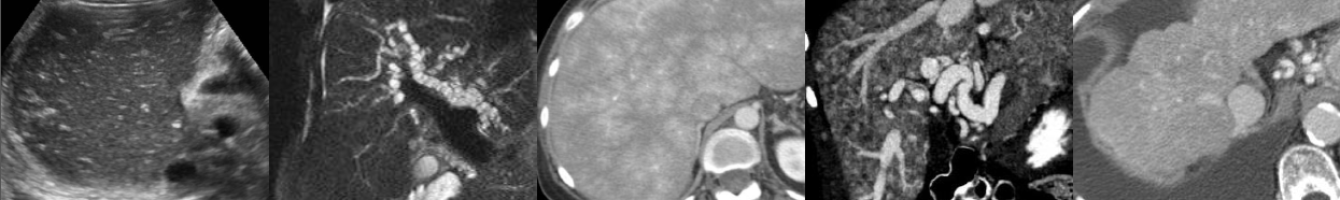
“Pancreatic cysts can be classi- fied into four subtypes: (a) unilocular cysts, (b) microcystic lesions, (c) macrocystic lesions, and (d) cysts with a solid component.”
Unilocular cysts: “Pseudocyst is the most common and the most frequently encountered cystic lesion in this group. Other less commonly encountered unilocular cysts include IPMNs, unilocular serous cystadenomas, and lymphoepithelial cysts.”
“Communication of the pseudocyst with the pancreatic duct may be seen at MR cholangiopancreatography or CT, especially on curved reformatted images. Cyst communication with the pancreatic duct can also be seen in IPMNs.”
“When present, multiple unilocular cysts are most often pseudocysts resulting from prior pancreatitis. Other causes of multiple cysts include von Hippel–Lindau disease and, rarely, IPMN. In von Hippel–Lindau disease, the pancreas is otherwise healthy and cysts may also be present in the kidneys or liver.”
“The only cystic lesion included in the category of microcystic lesions is serous cystadenoma. In 70% of cases, these benign tumors demonstrate a polycystic or microcystic pattern consisting of a collection of cysts (usually more than six) that range from a few millimeters up to 2 cm in size. A fibrous central scar with or without a characteristic stellate pattern of calcification is seen in 30% of cases and, when demonstrated at CT or MR imaging, is highly specific and is considered to be virtually pathognomonic for serous cystadenoma. The macrocystic or oligocystic variant of these tumors is very uncommon and is seen in less than 10% of cases.”
Macrocystic lesions: “The cystic tumors in this category include mucinous cystic neoplasms and IPMNs. Mucinous cystic neoplasms (mucinous cystadenomas) predominantly involve the body and tail of the pancreas.”
“Although peripheral eggshell calcification is not frequently seen at CT, such a finding is specific for a mucinous cystic neoplasm and is highly predictive of malignancy.”
“IPMNs can be classified as main duct, branch duct (side-branch), or mixed IPMNs. It is important to be aware that lack of communication with the main pancreatic duct at imaging does not exclude an IPMN.”
“The occurrence of malignancy is significantly higher in main duct and mixed IPMNs than in side-branch IPMNs.”
“Solid tumors associated with a cystic component include islet cell tumor, solid pseudopapillary tumor, adenocarcinoma of the pancreas, and metastasis.”
- International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas Key Points
“Worrisome features on imaging include cyst of 3 cm, thickened enhanced cyst walls, MPD size of 5-9 mm, non-enhanced mural nodules, abrupt change in the MPD caliber with distal pancreatic atrophy, and lymphadenopathy. Cysts with obvious high-risk stigmata on CT or MRI (i.e., obstructive jaundice in a patient with a cystic lesion of the pancreatic head, enhanced solid component, MPD size of 10 mm) should undergo resection without further testing. All smaller cysts with worrisome features should be evaluated by EUS to further risk-stratify the lesion. Patients with cysts of >3 cm and no worrisome features can also be considered for EUS to verify the absence of thickened walls or mural nodules, particularly if the patient is elderly. All patients with cysts of 3 cm in size without worrisome features should undergo surveillance according the size stratification.”
- Pancreatic Ductal Adenocarcinoma Radiology Reporting Template: Consensus Statement of the Society of Abdominal Radiology and the American Pancreatic Association