GI – Biliary
- Diffuse Gallbladder Wall Thickening: Differential Diagnosis Key Points
“[A thick-walled gallbladder], however, is not pathognomonic, and additional imaging signs should be present to support the diagnosis of acute calculous cholecystitis, such as an obstructing gallstone, hydropic dilatation of the gallbladder a positive sonographic ‘Murphy’s’ sign (i.e., pain elicited by pressure over the sonographically located gallbladder), pericholecystic fat inflammation or fluid, and hyperemia of the gallbladder wall at power Doppler imaging.”
“Acute acalculous cholecystitis mainly occurs in critically ill patients presumably because of increased bile viscosity from fasting and taking medication that causes cholestasis.”
“Imaging studies [or xanthogranulomatous cholecystitis] show marked gallbladder wall thickening, with the wall often containing nodules that are hypoechoic at sonography and hypoattenuating at CT; these nodules are abscesses or foci of xanthogranulomatous inflammation.”
“Porcelain gallbladder has been associated with gallbladder carcinoma; however, this association appears to be weak.”
“Gallbladder carcinoma has various imaging appearances, ranging from a polypoid intraluminal lesion to an infiltrating mass replacing the gallbladder, and it may also present as diffuse mural thickening.”
“MRI may be able to differentiate adenomyomatosis from gallbladder carcinoma by depicting Rokitansky-Aschoff sinuses.”
“Systemic diseases, such as liver dysfunction, heart failure, or kidney failure, may lead to diffuse gallbladder thickening.”
- MR Imaging of the Gallbladder: A Pictorial Essay
- Mimics of Cholangiocarcinoma: Spectrum of Disease
- Radiologic Manifestations of Sclerosing Cholangitis with Emphasis on MR Cholangiopancreatography
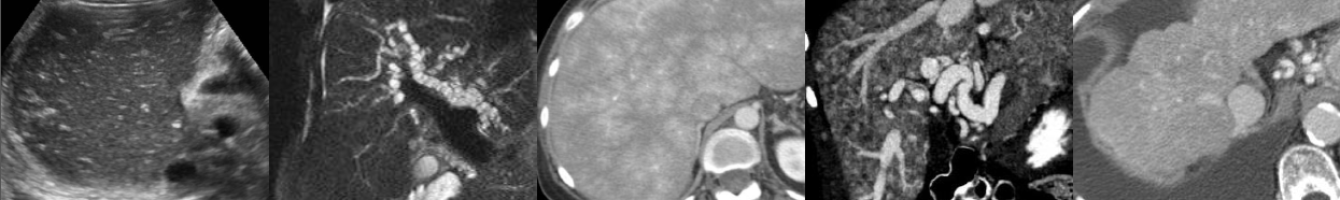
- Recurrent Pyogenic Cholangitis: From Imaging to Intervention Key Points
“Also known as oriental cholangiohepatitis, recurrent pyogenic cholangitis is a complex disease that is characterized by intrahepatic pigmented stones and recurrent attacks of cholangitis.”
“Although its exact cause is not known, there are strong associations between recurrent pyogenic cholangitis and parasites such as Ascaris lumbricoides and Clonorchis sinensis. It has been postulated that chronic infestation of the biliary tree by parasitic organisms induces inflammatory and fibrotic changes in the bile duct walls, leading to stricture formation, bile stasis, and intrahepatic stones. Men and women are affected with equal incidence, most frequently in the third and fourth decades of life.”
“The intrahepatic calculi lead to progressive biliary obstruction and recurrent infection, which in turn can result in multiple cholangitic hepatic abscesses; further biliary strictures; and, in severe cases, progressive hepatic parenchymal destruction, cirrhosis, and portal hypertension.” Complications: Hepatic abscess, biloma, PV thrombosis, malignancy (chlangiocarcinoma, HCC secondary to cirrhosis).
“Characteristically, there is disproportionate dilatation of the extrahepatic and central intrahepatic ducts, with little if any dilatation of the more peripheral biliary ducts. Pneumobilia…is also a common finding in recurrent pyogenic cholangitis. Hepatolithiasis is easier to detect on unenhanced CT because 90% of the stones are hyperdense to normal unenhanced liver parenchyma.”
“Hepatic parenchymal atrophy is a common feature of recurrent pyogenic cholangitis. It occurs most frequently in the left lateral segments, with the right posterior segments next most commonly involved.”
Although diffusion-weighted MRI has been shown to improve the detection of liver lesions and may have some role in the imaging of recurrent pyogenic cholangitis patients, it does not appear to confer any advantage in the differentiation of benign from malignant pathologic processes.”
“Therapeutic options for patients with recurrent pyogenic cholangitis include antibiotic therapy for acute attacks, stricture dilatation, biliary drainage, stone removal, biliary bypass, liver resection, and trans plantation. The goal of therapy is to completely clear the biliary tree of calculi and to eliminate bile stasis to prevent acute attacks of cholangitis and further stone formation. Where possible, patients are treated relatively conservatively using ERCP or PTC to achieve these goals, with surgical management reserved for those patients in whom endoscopic and percutaneous techniques have been unsuccessful.”
- Hepatobiliary and Pancreatic MRI and MRCP Findings in Patients with HIV Infection