GI
GI – Bowel
- Algorithmic Approach to CT Diagnosis of the Abnormal Bowel Wall Key Points
“The water halo sign indicates stratification within a thickened bowel wall that consists of either two or three continuous, symmetrically thickened layers. Common diagnoses with this sign include idiopathic inflammatory bowel diseases, vascular disorders, infectious diseases, and radiation damage.”
“The water halo sign is used as a generic term to indicate stratification within a thickened bowel wall that consists of either two or three continuous, symmetrically thickened layers. A halo sign with two layers (double halo) is composed of either a higher-attenuation outer annular ring (muscularis propria) surrounding a second, luminally oriented annular ring of gray attenuation or a higher-attenuation inner layer and an outer ring of gray attenuation. A third variant, the target sign, is composed of three rings: outer high-attenuation muscularis propria, a middle ring of gray attenuation, and a luminally oriented ring of high attenuation. The lower-attenuation (gray) layer of the water halo sign is believed to represent edema (thought to be its dominant component) and can be assumed to be located in the submucosa.”
“The water halo sign is most valuable as an unequivocal observation of bowel wall injury, often of an acute nature. Furthermore, although a myriad of small or large bowel pathologic conditions can produce these signs, malignancy rarely manifests with the classic water halo sign.”
“The fat halo sign refers to a three-layered target sign of thickened bowel in which the middle or “submucosal” layer has a fatty attenuation. Common diagnoses with this sign include Crohn disease in the small intestine and idiopathic inflammatory bowel diseases in the colon.”
“Pitfalls: Intramural fat may exist in both the distal ileum and colon as a “normal” variant in patients without gastrointestinal symptoms or a history of gastrointestinal disease. In the small intestine, normal intramural fat is seen most commonly in the terminal ileum. In the colon, it is found most often in the descending colon.”
“The normal intramural fat layer is generally very thin, usually thinner than the fat stratum. The observation of the normal fat halo sign is most frequently made in undistended or poorly distended bowel loops.”
- CT Findings in Adult Celiac Disease
- CT and MR Imaging Findings of Bowel Ischemia from Various Primary Causes
- Stercoral Colitis Leading to Fatal Peritonitis: CT Findings Key Points
“Fecal impaction may lead to ischemic pressure necrosis and subsequent colonic perforation. In the appropriate clinical setting, the imaging findings that should prompt the radiologist to consider this diagnosis are the presence of fecal impaction, focal colonic wall thickening, and adjacent stranding of the fat. If the fecal impaction is not promptly relieved, the condition can lead to colonic perforation, peritonitis, and patient demise.”
“The physiology of stercoral colitis is related to the development of a fecaloma, which is a conglomeration of dehydrated fecal material. This causes distention of the colonic lumen and increases the pressure on the wall, which decreases blood supply to the area. If not treated aggressively with cathartics, enemas, and/or manual disimpaction, the ischemia can lead to ulceration and perforation.”
- MR Imaging Evaluation of Perianal Fistulas: Spectrum of Imaging Features
- Mesenteric Adenitis: CT Diagnosis of Primary Versus Secondary Causes, Incidence, and Clinical Signficance in Pediatric and Adult Patients Key Points
“Mesenteric adenitis was considered present if a cluster of three or more lymph nodes measuring 5 mm or greater each was present in the right lower quadrant mesentery. If no other abnormality was detected on CT, then mesenteric adenitis was considered primary. If a specific inflammatory process was detected in addition to the lymphadenopathy, then mesenteric adenitis was considered secondary.”
“Mesenteric adenitis can be divided into two broad categories, primary and secondary. Primary mesenteric adenitis has been defined as right-sided mesenteric lymphadenopathy without an identifiable acute inflammatory process or with mild wall thickening of the terminal ileum.”
“In most cases of primary mesenteric adenitis, an underlying infectious terminal ileitis is thought to be the cause.”
“First, right lower quadrant mesenteric nodes do not occur in the general, asymptomatic, immunocompetent adult population. Second, an isolated cluster of right lower quadrant mesenteric lymph nodes is an uncommon finding in patients with acute abdominal symptoms, and this finding is often associated with a focal inflammatory process. Third, CT detection of right lower quadrant mesenteric nodes in patients with acute abdominal pain is usually associated with a detectable intraperitoneal inflammatory process in the majority of patients. Failure to identify a concurrent pathologic process leads to a presumptive diagnosis of primary mesenteric adenitis and explains the patient’s symptoms.”
GI – Anorectal Staging
- MR Imaging for Preoperative Evaluation of Primary Rectal Cancer: Practical Considerations Key Points
“High-resolution T2-weighted imaging is the key sequence in the magnetic resonance (MR) imaging evaluation of primary rectal cancer. This sequence generally consists of thin-section (3-mm) axial images obtained orthogonal to the tumor plane, with an in-plane resolution of 0.5–0.8 mm.”
“This technique allows differentiation between rectal tumors confined within the rectal wall (stage T2 tumors) and those that extend beyond the muscularis propria (stage T3 tumors). Most important, the depth of invasion outside the muscularis propria can be assessed with a high degree of accuracy. In addition, high-resolution T2-weighted images allow the morphologic assessment of pelvic nodes, thereby improving accuracy in the characterization of nodes as benign or malignant, since size criteria have proved to be of limited value.”
“Even with TME (total mesorectal excision), however, the presence of a tumor or malignant node within 1 mm of the CRM (circumferential reference margin) remains an important predisposing factor for local recurrence.”
“These studies also revealed that radiation therapy yields little survival benefit and results in significant morbidity when used to treat stage T1–T2 or favorable-risk early stage T3 tumors (<5 mm invasion outside the muscularis propria) in contrast to more advanced stage T3 tumors (>5 mm invasion outside the muscularis propria)”
“Recent studies have shown that high-resolution MR imaging is a reliable and reproducible technique with high specificity (92%) for predicting a negative CRM, the relationship of the tumor to the CRM, and the depth of tumor invasion outside the muscularis propria.”
“On T2-weighted images, stage T1 tumors are confined to the submucosa, which manifests as a hyperintense layer; stage T2 tumors extend into, but not beyond, the muscularis propria, which manifests as a hypointense layer; and stage T3 tumors extend beyond the muscularis propria into the mesorectal fat.”
“A distance greater than 1 mm between the tumor and the CRM at histopathologic examination has been shown to correlate with a decrease in local recurrence. At our institution, we consider a measured distance of 1 mm or less on high-resolution T2-weighted images to be indicative of CRM involvement. It is critical to remember that this measured distance is the distance to the mesorectal fascia from either (a) the tumor margin, (b) a tumor deposit in the mesorectum, (c) tumor thrombus within a vessel, or (d) a malignant node.”
“If a malignant node or tumor deposit abuts (ie, is less than 1 mm from) the mesorectal fascia, this information is important to the surgeon, who must stay well clear of the tumor at that margin. In the United States, nodes outside the mesorectal fascia along the pelvic sidewall are not routinely resected. However, if involvement of these nodes can be established preoperatively, it is important to modify the treatment approach to avoid recurrence in untreated nodes. Involved extramesorectal lymph nodes can be targeted with a widened field for preoperative radiation therapy and extended surgical resection.”
“It is well established that nodal size is of limited value in assessing for the presence of metastasis. The most frequently used size criterion for distinguishing malignant from nonmalignant nodes (ie, 5 mm) has a sensitivity of 68% and a specificity of about 78%. The limited accuracy of nodal size is likely related to the fact that 30%–50% of metastases in rectal cancer occur in nodes that are less than 5 mm. Recently, it was reported that nodal margins and internal nodal characteristics are the most reliable indicators of malignancy. Features that are suggestive of malignancy include irregular or spiculated nodal margins and heterogeneous signal intensity.”
- Imaging of Anal Carcinoma Key Points
“The most significant landmark of the anal canal is the dentate line, which lies 2.5–3 cm proximal to the anal verge and is visible macroscopically but not on MRI. Its position can be estimated either by measuring 2.5 cm above the anal verge or by dividing the anal canal into thirds so that the dentate line lies at the junction of the middle and upper thirds.”
“At initial staging, most tumors are T1 or T2, lie within 1.5 cm of the anal verge, have a circumferential extent of less than 50%, and are located predominantly along the anterior aspect of the anal canal.”
“The sphincter complex is the most commonly infiltrated structure, followed by the rectum. It should be emphasized that direct invasion of the rectal wall, perianal skin, subcutaneous tissues, or sphincter muscles does not signify a T4 tumor. Invasion of organs such as the vagina, urethra, prostate, or bladder is required to diagnose T4 disease.”
“MRI is especially useful in staging large tumors, particularly when the craniocaudal dimension is the largest dimension or when tumors protrude beyond the anal verge, because endoscopy is inadequate in these cases.”
“Nodal drainage depends on which side of the dentate line the anal cancer has its epicenter. Anal margin and anal canal tumors inferior to the dentate line spread to the inguinal and femoral lymph nodes, whereas anal canal tumors superior to the dentate line drain into the perirectal, internal iliac, and retroperitoneal nodes.
- MRI and CT of anal carcinoma: a pictorial review Key Points
“Nodal staging evaluation relies on the distance from the primary tumour rather than on the number of involved nodes. MRI is highly helpful to assess lymph node metastatic involvement, although the mere size criterion is far from accurate and associated with both false-positive and false-negative results. Short-axis threshold values of 8 mm, 5 mm and 10 mm have been suggested for pelvic, perirectal and inguinal lymph nodes, respectively. Additional helpful features to increase specificity include loss of the normal bean-shaped morphology and fatty hilum, internal T1 and T2 signal heterogeneity with central necrosis, and inhomogeneous enhancement.”
GI – Fluoroscopy
- Diseases of the Esophagus: Diagnosis with Esophagography
- Radiologic Diagnosis of Benign Esophageal Strictures: A Pattern Approach
- Double-Contrast Upper Gastrointestinal Radiography: A Pattern Approach for Diseases of the Stomach
- Pattern Approach for Diseases of Mesenteric Small Bowel on Barium Studies
- Double-Contrast Barium Enema Examination Technique
GI – Liver
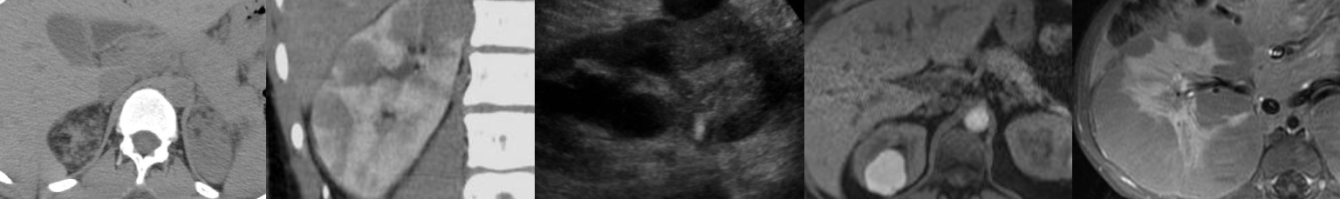
- Hypervascular Liver Lesions on MRI
- Focal Hepatic Lesions: Diagnostic Value of Enhancement Pattern Approach with Contrast-enhanced 3D GRE MR Imaging
- Dual Gradient-Echo In-Phase and Opposed-Phase Hepatic MR Imaging: A Useful Tool for Evaluating More Than Fatty Infiltration or Fatty Sparing
- LI-RADS: A Case-based Review of the New Categorization of Liver Findings in Patients with End-Stage Liver Disease Key Points
“[Focal perfusion alterations] are areas of arterial phase hyperenhancement most frequently caused by nontumorous arterioportal shunts or focal obstruction of a parenchymal portal vein branch. These alterations are usually peripheral, wedge shaped, and isointense relative to the surrounding parenchyma on T1- and T2-weighted MR images, and can be confidently characterized as LR-1; however, perfusion alterations can occasionally be nodular in contour and difficult to distinguish from a true enhancing lesion. Areas of nodular arterial phase hyperenhancement seen exclusively during the arterial phase are more appropriately categorized as LR-2, but if corresponding abnormalities (eg, increased T2 signal) can be seen on unenhanced images or with other sequences, perfusion alterations are considered unlikely, and the observation should be categorized as either LR-3 or LR-4 depending on its size and nonvascular features.”
- The Focal Hepatic Hot Spot Sign Key Points
“In the presence of superior vena cava obstruction, the left hepatic lobe may occasionally demonstrate areas of focally increased blood flow in the collateral veins that can be seen on images. Typically, the collateral venous pathway comprises the internal mammary vein that connects to the left portal vein via the paraumbilical vein.”
“The flow of blood through the collateral veins may result in areas of focally increased blood flow to the liver. Specifically, an area of increased activity in segment IV of liver (ie, within the medial segment of the left hepatic lobe in what was formerly known as the quadrate lobe) has been well documented in patients with superior vena cava obstruction; this area of increased activity can be seen on 99mTc–sulfur colloid scans of the liver and spleen and is referred to as the focal hepatic hot spot sign. The equivalent of this sign may also be seen on contrast material–enhanced computed tomographic (CT) scans.”
“Some other causes of hepatic hot spots include Budd-Chiari syndrome, liver abscess, hemangioma, focal nodular hyperplasia, and hepatocellular carcinoma. With the exception of Budd-Chiari syndrome, which causes the hot spot sign to occur in the caudate lobe, all other entities can cause the hot spot sign to occur anywhere in the liver, including segment IV.”
GI – Biliary
- Longitudinal Ultrasound Assessment of Changes in Size and Number of Incidentally-Detected Gallbladder Polyps
- Diffuse Gallbladder Wall Thickening: Differential Diagnosis Key Points
[A thick-walled gallbladder], however, is not pathognomonic, and additional imaging signs should be present to support the diagnosis of acute calculous cholecystitis, such as an obstructing gallstone, hydropic dilatation of the gallbladder a positive sonographic “Murphy’s” sign (i.e., pain elicited by pressure over the sonographically located gallbladder), pericholecystic fat inflammation or fluid, and hyperemia of the gallbladder wall at power Doppler imaging.”
“Acute acalculous cholecystitis mainly occurs in critically ill patients presumably because of increased bile viscosity from fasting and taking medication that causes cholestasis.”
“Imaging studies [or xanthogranulomatous cholecystitis] show marked gallbladder wall thickening, with the wall often containing nodules that are hypoechoic at sonography and hypoattenuating at CT; these nodules are abscesses or foci of xanthogranulomatous inflammation.”
“Porcelain gallbladder has been associated with gallbladder carcinoma; however, this association appears to be weak.”
“Gallbladder carcinoma has various imaging appearances, ranging from a polypoid intraluminal lesion to an infiltrating mass replacing the gallbladder, and it may also present as diffuse mural thickening.”
“MRI may be able to differentiate adenomyomatosis from gallbladder carcinoma by depicting Rokitansky-Aschoff sinuses.”
“Systemic diseases, such as liver dysfunction, heart failure, or kidney failure, may lead to diffuse gallbladder thickening.”
- MR Imaging of the Gallbladder: A Pictorial Essay
- Mimics of Cholangiocarcinoma: Spectrum of Disease
- Radiologic Manifestations of Sclerosing Cholangitis with Emphasis on MR Cholangiopancreatography
- Recurrent Pyogenic Cholangitis: From Imaging to Intervention Key Points
“Also known as oriental cholangiohepatitis, recurrent pyogenic cholangitis is a complex disease that is characterized by intrahepatic pigmented stones and recurrent attacks of cholangitis.”
“Although its exact cause is not known, there are strong associations between recurrent pyogenic cholangitis and parasites such as Ascaris lumbricoides and Clonorchis sinensis. It has been postulated that chronic infestation of the biliary tree by parasitic organisms induces inflammatory and fibrotic changes in the bile duct walls, leading to stricture formation, bile stasis, and intrahepatic stones. Men and women are affected with equal incidence, most frequently in the third and fourth decades of life.”
“The intrahepatic calculi lead to progressive biliary obstruction and recurrent infection, which in turn can result in multiple cholangitic hepatic abscesses; further biliary strictures; and, in severe cases, progressive hepatic parenchymal destruction, cirrhosis, and portal hypertension.” Complications: Hepatic abscess, biloma, PV thrombosis, malignancy (chlangiocarcinoma, HCC secondary to cirrhosis).
“Characteristically, there is disproportionate dilatation of the extrahepatic and central intrahepatic ducts, with little if any dilatation of the more peripheral biliary ducts. Pneumobilia…is also a common finding in recurrent pyogenic cholangitis. Hepatolithiasis is easier to detect on unenhanced CT because 90% of the stones are hyperdense to normal unenhanced liver parenchyma.”
“Hepatic parenchymal atrophy is a common feature of recurrent pyogenic cholangitis. It occurs most frequently in the left lateral segments, with the right posterior segments next most commonly involved.”
Although diffusion-weighted MRI has been shown to improve the detection of liver lesions and may have some role in the imaging of recurrent pyogenic cholangitis patients, it does not appear to confer any advantage in the differentiation of benign from malignant pathologic processes.”
“Therapeutic options for patients with recurrent pyogenic cholangitis include antibiotic therapy for acute attacks, stricture dilatation, biliary drainage, stone removal, biliary bypass, liver resection, and trans plantation. The goal of therapy is to completely clear the biliary tree of calculi and to eliminate bile stasis to prevent acute attacks of cholangitis and further stone formation. Where possible, patients are treated relatively conservatively using ERCP or PTC to achieve these goals, with surgical management reserved for those patients in whom endoscopic and percutaneous techniques have been unsuccessful.”
- Hepatobiliary and Pancreatic MRI and MRCP Findings in Patients with HIV Infection
GI – Pancreas
- Cystic Pancreatic Lesions: A Simple Imaging-based Classification System for Guiding Management Key Points
“Pseudocysts, serous cystadenomas, mucinous cystic neoplasms, and IPMNs are most often encountered in routine practice, accounting for more than 90% of cystic pancreatic lesions. Pseudocysts typically occur with acute pancreatitis or may develop insidiously in the setting of chronic pancreatitis.”
“Pancreatic cysts can be classi- fied into four subtypes: (a) unilocular cysts, (b) microcystic lesions, (c) macrocystic lesions, and (d) cysts with a solid component.”
Unilocular cysts: “Pseudocyst is the most common and the most frequently encountered cystic lesion in this group. Other less commonly encountered unilocular cysts include IPMNs, unilocular serous cystadenomas, and lymphoepithelial cysts.”
“Communication of the pseudocyst with the pancreatic duct may be seen at MR cholangiopancreatography or CT, especially on curved reformatted images. Cyst communication with the pancreatic duct can also be seen in IPMNs.”
“When present, multiple unilocular cysts are most often pseudocysts resulting from prior pancreatitis. Other causes of multiple cysts include von Hippel–Lindau disease and, rarely, IPMN. In von Hippel–Lindau disease, the pancreas is otherwise healthy and cysts may also be present in the kidneys or liver.”
“The only cystic lesion included in the category of microcystic lesions is serous cystadenoma. In 70% of cases, these benign tumors demonstrate a polycystic or microcystic pattern consisting of a collection of cysts (usually more than six) that range from a few millimeters up to 2 cm in size. A fibrous central scar with or without a characteristic stellate pattern of calcification is seen in 30% of cases and, when demonstrated at CT or MR imaging, is highly specific and is considered to be virtually pathognomonic for serous cystadenoma. The macrocystic or oligocystic variant of these tumors is very uncommon and is seen in less than 10% of cases.”
Macrocystic lesions: “The cystic tumors in this category include mucinous cystic neoplasms and IPMNs. Mucinous cystic neoplasms (mucinous cystadenomas) predominantly involve the body and tail of the pancreas.”
“Although peripheral eggshell calcification is not frequently seen at CT, such a finding is specific for a mucinous cystic neoplasm and is highly predictive of malignancy.”
“IPMNs can be classified as main duct, branch duct (side-branch), or mixed IPMNs. It is important to be aware that lack of communication with the main pancreatic duct at imaging does not exclude an IPMN.”
“The occurrence of malignancy is significantly higher in main duct and mixed IPMNs than in side-branch IPMNs.”
“Solid tumors associated with a cystic component include islet cell tumor, solid pseudopapillary tumor, adenocarcinoma of the pancreas, and metastasis.”
- International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas Key Points
“Worrisome features on imaging include cyst of 3 cm, thickened enhanced cyst walls, MPD size of 5-9 mm, non-enhanced mural nodules, abrupt change in the MPD caliber with distal pancreatic atrophy, and lymphadenopathy. Cysts with obvious high-risk stigmata on CT or MRI (i.e., obstructive jaundice in a patient with a cystic lesion of the pancreatic head, enhanced solid component, MPD size of 10 mm) should undergo resection without further testing. All smaller cysts with worrisome features should be evaluated by EUS to further risk-stratify the lesion. Patients with cysts of >3 cm and no worrisome features can also be considered for EUS to verify the absence of thickened walls or mural nodules, particularly if the patient is elderly. All patients with cysts of 3 cm in size without worrisome features should undergo surveillance according the size stratification.”
- Pancreatic Ductal Adenocarcinoma Radiology Reporting Template: Consensus Statement of the Society of Abdominal Radiology and the American Pancreatic Association
Abdominal MRI Physics