“High-resolution T2-weighted imaging is the key sequence in the magnetic resonance (MR) imaging evaluation of primary rectal cancer. This sequence generally consists of thin-section (3-mm) axial images obtained orthogonal to the tumor plane, with an in-plane resolution of 0.5–0.8 mm.”
“This technique allows differentiation between rectal tumors confined within the rectal wall (stage T2 tumors) and those that extend beyond the muscularis propria (stage T3 tumors). Most important, the depth of invasion outside the muscularis propria can be assessed with a high degree of accuracy. In addition, high-resolution T2-weighted images allow the morphologic assessment of pelvic nodes, thereby improving accuracy in the characterization of nodes as benign or malignant, since size criteria have proved to be of limited value.”
“Even with TME (total mesorectal excision), however, the presence of a tumor or malignant node within 1 mm of the CRM (circumferential reference margin) remains an important predisposing factor for local recurrence.”
“These studies also revealed that radiation therapy yields little survival benefit and results in significant morbidity when used to treat stage T1–T2 or favorable-risk early stage T3 tumors (<5 mm invasion outside the muscularis propria) in contrast to more advanced stage T3 tumors (>5 mm invasion outside the muscularis propria)”
“Recent studies have shown that high-resolution MR imaging is a reliable and reproducible technique with high specificity (92%) for predicting a negative CRM, the relationship of the tumor to the CRM, and the depth of tumor invasion outside the muscularis propria.”
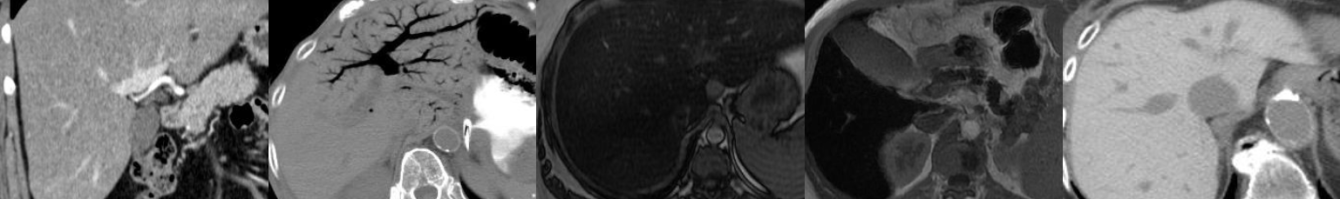
“On T2-weighted images, stage T1 tumors are confined to the submucosa, which manifests as a hyperintense layer; stage T2 tumors extend into, but not beyond, the muscularis propria, which manifests as a hypointense layer; and stage T3 tumors extend beyond the muscularis propria into the mesorectal fat.”
“A distance greater than 1 mm between the tumor and the CRM at histopathologic examination has been shown to correlate with a decrease in local recurrence. At our institution, we consider a measured distance of 1 mm or less on high-resolution T2-weighted images to be indicative of CRM involvement. It is critical to remember that this measured distance is the distance to the mesorectal fascia from either (a) the tumor margin, (b) a tumor deposit in the mesorectum, (c) tumor thrombus within a vessel, or (d) a malignant node.”
“If a malignant node or tumor deposit abuts (ie, is less than 1 mm from) the mesorectal fascia, this information is important to the surgeon, who must stay well clear of the tumor at that margin. In the United States, nodes outside the mesorectal fascia along the pelvic sidewall are not routinely resected. However, if involvement of these nodes can be established preoperatively, it is important to modify the treatment approach to avoid recurrence in untreated nodes. Involved extramesorectal lymph nodes can be targeted with a widened field for preoperative radiation therapy and extended surgical resection.”
“It is well established that nodal size is of limited value in assessing for the presence of metastasis. The most frequently used size criterion for distinguishing malignant from nonmalignant nodes (ie, 5 mm) has a sensitivity of 68% and a specificity of about 78%. The limited accuracy of nodal size is likely related to the fact that 30%–50% of metastases in rectal cancer occur in nodes that are less than 5 mm. Recently, it was reported that nodal margins and internal nodal characteristics are the most reliable indicators of malignancy. Features that are suggestive of malignancy include irregular or spiculated nodal margins and heterogeneous signal intensity.”